Staying strong through hardships
Claire Snyder was diagnosed with Acute Lymphocytic Leukemia on June 21, 2018. Now awaiting new cell growth after bone marrow transplant, the junior is excited and hopeful to live a cancer-free life.

Cancer. One simple word. A word no one wants to hear. A word to which one can only wince at in response. A diagnosis one can’t even imagine. So powerful yet so emptying, it’s sour stench leaves you breathless. No one expects it, that six letter word. That stealing, cruel word.
Claire Snyder, a junior at Lawrence North, was just like any average teenager. While also maintaining her grades, Claire was very active in school, taking part in the LN’s Girls Swim Team, and also playing an instrument for the school orchestra. When school let out for the summer, she hung out with friends and worked as a lifeguard at her local swimming pool. However, all of that came to an abrupt halt just weeks into break. On June 21, 2018, just weeks before her sixteenth birthday, Claire was diagnosed with B-cell Acute Lymphocytic Leukemia.
“It felt like someone had dropped a boulder on me,” Claire said.
Acute Lymphocytic Leukemia, also known as Acute Lymphoblastic Leukemia, is a type of cancer of the blood and bone marrow, stemming from early or immature forms of white blood cells, also called lymphocytes. In children with ALL, the white blood cells in the bone marrow do not mature how they are supposed to, meaning they can’t properly fulfill their job of fighting infection. Overcrowding of the lymphocytes can occur, not leaving much room for other healthy white blood cells, red blood cells and platelets. With red blood cells in charge of carrying oxygen and platelets in charge of forming blood clots, too few of these healthy cells present in the bone marrow can lead to high risk of infection, bleeding problems and anemia.
“I immediately looked up survival rates mostly to help my brother and sister know I’d probably be okay. I was just really hopeful at first and I still didn’t fully believe I had cancer until I got to the hospital and the doctor told me to my face,” Claire said.
Claire started to notice that something was off around two weeks prior to her diagnosis, which included a growing numbness in her lip as well as easy bruising that only seemed to be getting worse. Looking back afterwards, she also believes the symptoms were evident way earlier than she believed.
“I think one of my first symptoms was joint pain, back pain, and muscle soreness. But, you know, I’m tall and do a lot of exercise, so why wouldn’t I have joint pain? I was also just really tired all the time and when I didn’t get food, I would be in awful condition,” Claire said.
One morning, Claire woke up to petechiae, or little red patches, all over her body, confirming her previous suspicions and bringing her to the hospital a day later. Expecting a simple prognosis such as pneumonia, cancer was nowhere on Claire’s mind.
“After we got my bloodwork, we got KFC and I was eating my chicken and I heard my mom crying in the garage. She walked in crying, and I said ‘I better not have cancer,’ and she just nodded and cried and hugged me and explained to my brother, sister, and dad what had happened and everyone was just crying. I think that’s the most painful memory I have,” Claire said.
Almost immediately, Claire was admitted to the hospital where she began her chemotherapy treatment. For Claire, and for most ALL patients, this would be the beginning of Leukemia treatment, which usually consists of three phases: induction, consolidation, and maintenance, all with the end goal of remission.
The first phase, induction, usually lasts around a month, which can be very intense, requiring frequent doctor visits. Before beginning the chemotherapy, steroids are usually taken, followed by spinal taps towards the beginning and end of the phase as well as many different chemo drugs like Vincristine, Daunorubicin and many others.
“The worst though were the crazy fluctuations in my weight resulting in a lot of stretch marks. Then there was the hair loss which, once my steroid, cancer-chubby face went down, wasn’t so bad. The very worst part, though, was the peripheral neuropathy as a side effect from the Vincristine. It started out with numbness and tingling sensations. Then, one day, I woke up and I couldn’t fully open my left hand and my right hand was so bad that it literally shriveled up and I could do very very little with it,” Claire said.
Consolidation, the phase following induction, is a more intense continuation of the leukemia treatment, typically lasting around two months. Consisting of similar treatment, this phase is a continuation of the chemotherapy treatment, but more intense than the previous.
After three long months of doctor visits and chemotherapy treatments, maintenance therapy would have been the next step for Claire. However, because she had not yet reached remission, and because of her genes themselves, Claire and her team had to look into other options to further her treatment to effectively lower the count of cancer cells in her body and bring her closer to remission.
“For some people, it’s like their immune systems need a restart, so they can get a transplant with their old cells so they get rid of all their bad cells and get their other ones as their transplant. For me, the genetics of my actual stem cells are messed up so they will keep getting made messed up and unable to determine cancer cells. So if they gave me back my own cells, they would just keep doing the same thing they already were. Same with chemo, I would stay in remission as long as I still had chemo and then there would be a 70% chance of relapse for the rest of my life. The only option for me based on my genetics is to replace the entire system with one that will catch cancer cells when it sees them,” Claire said.
In closely approaching the beginning of the maintenance phase, it became clearer that the bone marrow transplant was the next best step for Claire on her way to becoming cancer free.
“I was meant to be in remission after each phase, meaning an undetectable MRD, which is technically just < 0.01% cancer cells because that’s the lowest they can see right now, but I wasn’t. So instead of continuing on with chemo that wasn’t working, and going into the maintenance stage, we chose to start prepping me for transplant instead with a specifically targeted drug called blinatumomab that would put me into temporary remission so that I could receive a transplant,” Claire said.
After a couple of months on high chemotherapy doses to temporarily bring her to remission, Claire would make the long trip to Cincinnati after many benchmark exams for her bone marrow transplant. On Jan. 21, Claire was admitted to the hospital where she tackled the necessary preparations for her transplant. Claire began the week-long preparation with four days of total body irradiation, which works to suppress the immune system and prevent rejection of the donor cells, followed by two days of chemotherapy as well.
“By now, food had lost flavor (that hasn’t stopped yet). My salivary glands were swollen and also didn’t produce enough spit to eat dry food. The first chemo day seemed easy but then I got really nauseous (this has improved) and started to get mucositis (this has got a lot worse). The whole prep week, I felt really fatigued and slept like 18 hours a day,” Claire said.
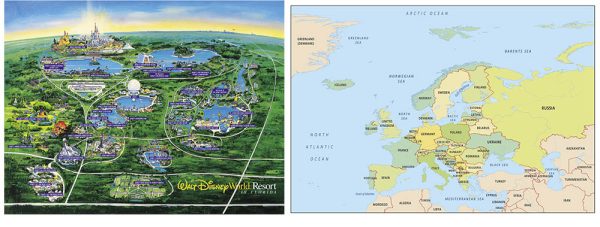
On Jan. 30, Claire’s donor cells arrived from Europe, with the total transplant being around six hours long. Similarly to a blood transfusion, the donated stem cells drip through a central line, moving through the bloodstream, eventually finding their way to the bone marrow.
“The genetics of her cancer put her at a greater than 70% chance of relapse unless she were to get a bone marrow transplant. The expectation is that this bone marrow transplant is a cure for her,” Claire’s mother April Snyder said.
After the transplant, the next step is to await the growth of the cells and to monitor to make sure growth and engraftment is occuring. Due to high risk of infection, Claire has to stay confined to her room at the hospital. Even after being discharged, Claire has to remain near the hospital until 100 days after having the transplant due to the fragile state of her immune system.
“I’m confined to my room and I have been for about a month now. Visitors are restricted and if I have to leave my room, we have to take back hallways and I have to wear a heavy duty mask because my immune system is still growing back from zero. When I’m discharged, it’ll be back to the same mask and food rules and avoiding people as much as possible,” Claire said.
During such a time, a strong support system is imperative to those being affected. Through this journey, Claire has learned that, more than ever, she has a great deal of friends and family who care for her and support her.
“I just want her to be happy. Obviously, being healthy is super important. But I hope she’s okay too, mentally, emotionally,” junior Zaheen Rashed said.
Throughout treatment, Claire’s family has played a big role in helping her through treatment. Though Claire may not be able to see her all of her loved ones at all times, support is present, however expressed.
“My family through has had to literally support me, even physically for a little bit, because when I was laying in bed and couldn’t sit up for more than a few seconds, my mom would cook me breakfast every morning and make me ginger tea which helps with nausea. And my extended family all reaches out in their churches and people were always sending me things like cookies, money, meals and just fun packages they thought I would enjoy. And all my friends have been super awesome and they haven’t treated me any differently. They’re really good friends, and some of them just recently sent me this huge basket with so many nice notes and gifts and it was really nice.”
Despite all of the ups and downs through treatment, Claire and her family remain positive and are hopeful for the future and excited for a healthy and cancer-free life.
“We are blessed that she had a perfect match and we pray that these new stem cells take good care of her for the rest of her very long life. We have no doubt that she will be back to school, swimming, driving, college visits, and everything else she’s looking forward to doing,” April Snyder said.









Kevin Thomasson • Mar 2, 2019 at 10:43 pm
That was a great story. I’m glad that Claire has friends like this who took the time to write this story.